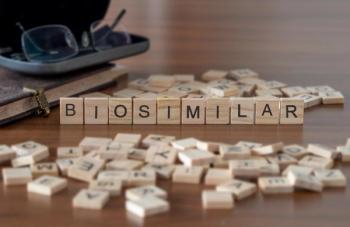
Using Secondary Patents and Skinny Labels
The impact on biosimilar utilization in clinical practice caused by secondary patents of biologics and skinny labels of biosimilars is discussed.
Episodes in this series
Bhavesh Shah, RPh, BCOP: One last thing I want to talk about is implications of secondary patents and what a skinny label is—that’s the term we hear in the current market. Brandon, I would like to understand your explanation on that.
Brandon Dyson, PharmD, BCOP, BCPS: If you’re a drug manufacturer of the originator biologic product, you have a goal to maintain patent rights on your drug for as long as possible. If you’re a biosimilar company trying to create a biosimilar, you have a goal to get it to market as cost-effectively as possible. I think of secondary patents and skinny labels as the 2 of the tools that each side has at its disposal. A secondary patent is when you make a change in formulation of an existing product, which can change how it’s delivered. It can change any number of things, and then you get a patent on that. A good example of this might be the Neulasta [pegfilgrastim] on-body injector. There are biosimilars for Neulasta [pegfilgrastim] for the syringe, but not for the on-body injector. They’ve been able to extend their patent by creating this different formulation.
Another thing you’re seeing more of recently is other drugs like rituximab and daratumumab, which have subcutaneous formulations. That is a secondary patent where they create it in a different dose form and are able to extend all the rights and privileges of rituximab, the originator product, in this new form. Skinny labels are on the other side; that’s what a biosimilar company might do. Rituximab actually is a fantastic example of this because rituximab is used for nearly a dozen rheumatoid conditions and B-cell lymphomas. It’s used in a lot of places. For example, Ruxience [rituximab] does not have on its package insert “rheumatoid arthritis.” They did not pursue that as part of their strategy. By doing that, I assume they have been able to save money on developing that particular thing on Ruxience [rituximab]. They’re able to get it to market in a more cost-effective way, and it may very well be used for rheumatoid arthritis because we use rituximab for rheumatoid arthritis. There can be interesting legal implications on this. Even recently, not in the biologic world, but there’s been ongoing debate with Coreg [carvedilol]—it’s actually still an ongoing piece of literature or piece of legislation—that, depending on how the courts decide how that ends up, could impact what skinny labels look like and if they’re advantageous or not.
Bhavesh Shah, RPh, BCOP: That’s a great summary. I also wanted to ask our panelists, does that have implications in your practice, having a drug with a skinny label? Brandon, perhaps you can answer that. Does that have any implications in how you utilize a biosimilar in your practice?
Brandon Dyson, PharmD, BCOP, BCPS: In a community setting, a lot of what steers our practice is payer driven. If a payer is unwilling to pay for something that’s not on the package insert, then it absolutely has an impact. We will not use that product. But many others and many times it does not. Many payers prefer biosimilars because it’s more cost-effective and because they do, as we’ve learned already, go through a high burden of proving they’re similar.
Bhavesh Shah, RPh, BCOP: Also to note, I think NCCN [National Comprehensive Cancer Network] Guidelines are also driven payer reimbursement. So having these indications in the NCCN Guidelines helps us with payer coverage. Payers will definitely be talking more about that. Tim, what biosimilars are currently approved from a therapeutics perspective in oncology?
Tim Peterson, PharmD, BCOP: From a therapeutic standpoint, our first biosimilar that was approved was the first of currently 2 approved bevacizumab biosimilars, and that was in 2017. As we know, our first biosimilar that was approved was in 2015 in the supportive care context with the first filgrastim. But since we started seeing the approval of our first bevacizumab therapeutic biosimilar, we’ve had 3 biosimilars FDA approved for rituximab. Now we’re up to 5 biosimilars approved for trastuzumab. As you might expect based on other discussions about biosimilars, not all these are available in the market because of numerous patent litigations and all these types of things that cause these significant delays. We’ve talked about rebate traps and that type of thing, which is another legislative discussion that’s certainly ongoing as far as I know. But that’s where we stand for therapeutics, and all 3 of those therapeutic monoclonal antibodies have additional biosimilars in the pipeline. Clearly, we’ll see some more coming from other targets as well.
Bhavesh Shah, RPh, BCOP: There are definitely more biosimilars for many of the approved biosimilars, so it’s really exciting to have this competition.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.