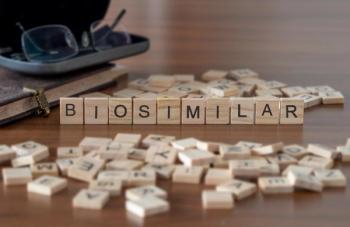
Challenges and Management of Adopting Biosimilars
Experts discuss managing biosimilar adoption in various clinical practice settings, working through the P&T (Pharmacy and Therapeutics) approval process, and the importance of relying on a shared-decision making framework.
Episodes in this series
Bhavesh Shah, RPh, BCOP: Brandon, in terms of the community side, what has that looked like for biosimilar adoption?
Brandon Dyson, PharmD, BCOP, BCPS: I’ll echo a bit of what Ryan said. We dipped our toes in cautiously. There may be a few reasons for that. In part, on the community side there are a lot of rebates direct from the manufacturers. You buy a couple of months’ supply of some drug, and you get an x-percent rebate. That happens across the practice. In some respects we may have had, for lack of a better term, a stockpile of brand originator product that we’ve got to get through before we decide anything. But the other thing is that it’s largely payer driven. It’s not that it’s all about the money. We want to give the patient the best-quality care, but we also can’t ask a patient to pay cash if their insurance is not willing to pay for the originator biologic product. A lot of our wading in started going with that. We started in a way that payer X said, “I need you to use this product instead.” When you’re facing that, we’re either not going to get paid for this or we got to use the biosimilar we started doing that. It went from there. It’s ballooned out, and now we’re very fluent with biosimilar use.
Bhavesh Shah, RPh, BCOP: That’s great. Tim, I know you guys get a lot of referrals from out of state. Many of your patients are not from the territory, and obviously we know that there are a lot of changes across state lines. How do you manage biosimilar adoption in a situation like that?
Tim Peterson, PharmD, BCOP: Thankfully we started our biosimilar pathway about a year and a half or 2 years ago. We are very lucky to have a lot of resources available both financial and personnel. We have a great patient financial services department that actually works in combination and coordination with our staff pharmacy. They perform prior authorizations ahead of time to identify the appropriate biosimilar or reference product for any individual situation, whether it’s rituximab, trastuzumab, or bevacizumab. All of them have a built-in pathway that, as I mentioned previously, is treated essentially as an “interchangeable process” for us that the financial services folks put in an order in our EMR [electronic medical record] to coordinate with the staff pharmacy to do that. This is entirely a pharmacy-driven process that’s been adopted by the entire institution.
Bhavesh Shah, RPh, BCOP:It seems that this is the trend. We see the success of biosimilar adoption has really been places where it’s driven by pharmacy. I’m curious about that process actually. We can help some of our audience members in terms of identifying a lot of those barriers that they could actually overcome with adopting a biosimilar with the P&T [pharmacy and therapeutics] process specifically. I’m going to call on you, Ryan, for that because you’ve championed this pretty well at your institution.
Ryan Haumschild, PharmD, MS, MBA: Thanks, but it’s still a work in progress. But to your point, you have to be strategic in the way you go about it. It’s not 1 size fits every institution. When we did the survey, we recognized there was some education needed but we also recognized that we need P&T approval to come up with pharmacy ownership of the process. That extends even into the EMR build, focusing on the question of how do we build it? Do we build out a preferred biosimilar with subsidiary biosimilar as a selection? Do we build out the generic drug name, such as rituximab, and then whatever biosimilar we choose based on payer need would be the right 1 on the back end and the pharmacy could do that independently. Those are some of the strategies that we’ve explored to be effective.
Through a clever practice agreement we have a lot of PGY1 [postgraduate year 1] and PGY2 [postgraduate year 2] board-certified oncology pharmacists and board-certified oncology pharmacists who work in our infusion center. It allows them to be a lot more agile. If precertification gets a kickback on our preferred biosimilar, they can easily send that over. Pharmacy can switch it, and provider really gets notified on the back end but doesn’t have to leave what they’re doing—seeing patients or on rounds—to be part of the process. It allows us to get that approval, the patient doesn’t feel any difference, and it’s a lot more streamlined. We’re reducing that total cost of care for not just our institution but also the patient. That’s been a huge win, Bhavesh, to your point, and leveraging that P&T–approved process has gone a long way.
Bhavesh Shah, RPh, BCOP: You guys are pretty big also on pathways and order set. Is that something that’s dictated by a pathway in your system? Electronic record? Is that built out that way?
Ryan Haumschild, PharmD, MS, MBA: You’re right. We try to hardwire it. We try to make it easy on everybody. It’s typically like those surveys that we fill out sometimes. If we miss 1 checkbox on the EMR, it won’t let us go to the next page. We have our order sets built the same way. Through a shared decision-making process from that disease group and also from the oncology P&T committee, we select the best product that meets our payroll requirements, contracting for our organization, and patient needs. That way, we already have it preselected so they can go ahead and launch that plan and follow that pathway, and everything flows from there. If they really want to select something different, there are some avenues that the providers can do. Most of the time they trust that shared decision-making framework to know that the right product was going to be there when they execute the plan.
Bhavesh Shah, RPh, BCOP: Brandon, what about on the community side? How do you guys go through the process, the checks and balances of getting a biosimilar onto formulary?
Brandon Dyson, PharmD, BCOP, BCPS: It’s pretty similar. It happens at the P&T level with physician and pharmacy leadership. They get together to evaluate the data, and they look at everything. I work with Texas Oncology, but we’re part of a larger national network called US Oncology. There’s a whole US Oncology P&T committee that helps make and drive these decisions. We don’t technically have a collaborative practice agreement, but it is a policy that once we’ve gone full in on whatever biosimilar, the physician can enter it. In the EMR it will default to the biosimilar. So he or she will have to click off it if they don’t want it for some reason. Two, we have the ability as pharmacists to switch on the spot without bothering for an order. There are instances when a brand might be preferred or when the originator might be preferred. There are avenues for that as well. In general, we try to make it easy, and it defaults to this and pharmacy can switch. If we have an authorization team and if they are seeking authorization, and the insurance kicks back and says, “I don’t want to use this. I want to use this other 1,” we can switch that too at the time without bothering anybody.
Bhavesh Shah, RPh, BCOP: It seems as though you guys also have a similar process.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.