Tumor Lysis and Chronic Lymphocytic Leukemia
Chronic lymphocytic leukemia experts debate how to prevent or reduce the risk of tumor lysis in patients.
Episodes in this series

Kirollos Hanna, PharmD, BCPS, BCOP: Let’s segue into an important concept: tumor lysis. You mentioned that these patients may have leukocytosis at baseline or come with a very high ALC [absolute lymphocyte count] and that ultimately, when you give therapies, they see leukocytosis, etc. When we talk about tumor lysis, the biggest drug we’re going to focus on is the BCL2 inhibitor venetoclax. For our listeners, when we talk about tumor lysis prevention, the patient at most risk is going to be that person on venetoclax. But when you look at the CLL14 and MURANO trials, the clinical incidence of TLS [tumor lysis syndrome] was 0%. With laboratory TLS, you had some changes in their lab parameters, so we saw very low numbers there. When you follow the appropriate titration schedule of venetoclax, it’s a 5-week titration and not the same as the AML [acute myeloid leukemia] dosing. That’s very important. Or if you debulk them with your anti-CD20 first as 1 of the approaches, that’s going to be very important and a key to success to lead to that 0 incidence of clinical TLS.
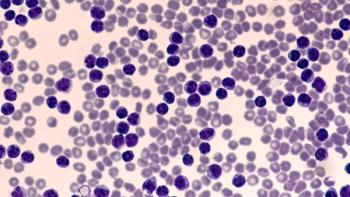
There are [some] things we have to focus on in terms of evaluating our patients for tumor lysis. What is their absolute lymphocyte count at baseline? What are their lymph node sizes at baseline? How many lymph nodes throughout their system do they have? What are their baseline laboratory parameters? [What does their] organ function look like? In terms of your absolute lymphocyte count, if you have a patient greater than 25,000, you’re probably going to treat that patient as a moderate-risk patient, potentially even a high-risk patient, if they have other factors that increase the risk for developing tumor lysis.
In terms of their lymph node size, there are 3 categories: 5 cm or less, 5 to 10 cm, and greater than 10 cm. How many of these lymph nodes are there? That’s going to be a clinical assessment call. If I have a patient with 3 or 4 lymph nodes, all 7 cm, I’m probably going to treat them as high risk, moderate risk, or on the higher end of moderate. Lastly are your baseline labs: what does the creatinine look like? What does the renal function look like? What does their baseline uric acid look like? Then [we look at] various electrolytes—your calcium, your phosphorus, your potassium. Based on these assessments, you’re able to put your patient in different buckets, whether it’s low risk for TLS, moderate or intermediate risk for TLS, or high risk for TLS.
Those higher-risk patients are the most concerning. Those are the patients you may consider admitting and treating with aggressive fluid hydration. If you have a high-baseline uric acid, maybe something like rasburicase prophylactically or right from the get-go with this patient population. All these patients are going to require antihyperuricemics with allopurinol. We’ll talk about pharmacy considerations later, but it’s also very important to avoid drug-drug interactions, especially during the ramp-up phase of venetoclax.
Your low-risk patients are on the other side of the spectrum, as long as they can stay hydrated, adhere to the ramp-up schedule, and adhere to their laboratory schedule. You’re going to have to evaluate labs more frequently as you’re ramping up, especially on those first days of each ramp-up level—sometimes predose, 6 to 8 hours in, 24 hours later—to make sure. If you’re high risk, you’re evaluating it much more frequently. In terms of tumor lysis syndrome, all these things are going to be very important considerations for your patients. Mr Perissinotti, is there anything different that you’d consider for TLS?
Anthony Perissinotti, PharmD, BCOP: No, you perfectly articulated all that. To summarize, you have patients who are high risk, intermediate risk, or low risk for TLS. For high-risk patients and some of your intermediate risk, unfortunately, you have to admit those patients for extra monitoring. There was an ASH [American Society of Hematology Annual Meeting] abstract based on the CLL13 trial, a study that had multiple arms—well, 3 arms had a venetoclax-based regimen. They did the trick that Mr Hanna talked about and did a lead-in with your anti-CD20 monoclonal. They did about 3 doses of obinutuzumab or obinutuzumab with ibrutinib before starting venetoclax. They ended up finding is that a substantial number of patients were able to be reduced from that high-risk category down to intermediate, and some intermediates down to low risk. What that means clinically is probably nothing. As Mr Hanna said, the risk for TLS is still pretty low based on our dose escalation. What that means logistically is that you no longer have to admit your patient into the hospital to administer their first dose and then the second week of their dose escalation of venetoclax. I like how we now have data from CLL13 that this strategy is effective.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.