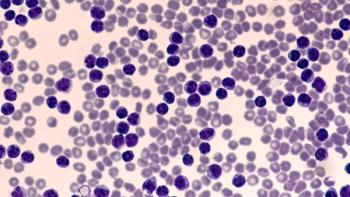
Second-Generation BTK Inhibitors for Chronic Lymphocytic Leukemia
Kirollos Hanna, PharmD, BCPS, BCOP, discusses clinical trial data for second-generation BTK inhibitors for chronic lymphocytic leukemia.
Episodes in this series

Anthony Perissinotti, PharmD, BCOP: Now we have some new kids on the block, our second-generation BTK [Bruton tyrosine kinase] inhibitors: acalabrutinib and zanubrutinib. Dr Hanna, I know there’s been quite a bit of data previously published, but also more data at ASH [American Society of Hematology annual meeting 2021] that are trying to help us discern, should we continue to use ibrutinib or should we jump ship and start using the second generation? What data were you most compelled by, and what is the role now with the second-generation BTK inhibitors?
Kirollos Hanna, PharmD, BCPS, BCOP: That’s a really good question, Dr Perissinotti. I think when we talk about this, the landscape has become extremely crowded with our BTK inhibitors, whether we’re talking about ibrutinib, acalabrutinib or zanubrutinib. But what really excites me is that CLL [chronic lymphocytic leukemia] doesn’t mimic a lot of the trends that we’ve seen in many cancers. We actually have head-to-head trials now comparing some of the BTK inhibitors. So when we start having discussions in clinical practice in terms of which drug selection should we go with based on my patient, there are a lot of factors that we do have to consider. I do think that it is important for us, outside of ibrutinib, though, very quickly, to talk a little about the long-term follow-up data from both the other BTK inhibitors that are available. We know that acalabrutinib is FDA approved, and zanubrutinib is not yet FDA approved, but it’s certainly mentioned in the NCCN [National Comprehensive Cancer Network] guidelines, and they’re also working on a potential FDA approval. So it’s really exciting for us to look at that.
What we saw at ASH, one of the notable trials is looking at ASCEND. When we talk about the ASCEND trial in terms of acalabrutinib, this was a randomized multicenter, open-label, phase 3 trial. It looked at patients with relapsed or refractory CLL, so they were already pretreated, probably with chemoimmunotherapy, and then they went on to either receive acalabrutinib or investigator’s choice of combination idelalisib plus rituximab, so combination PI3K plus anti-CD20, or bendamustine, rituximab. They wanted to see, does that acalabrutinib component have benefit for these patients over PI3K, anti-CD20, or chemoimmunotherapy? And what we saw in this trial, in terms of long-term follow-up, at 36 months, the progression-free survival [PFS] rates were much higher, statistically significantly higher, in the patients who received acala [acalabrutnib] vs IdR [idelalisib plus rituximab], or BR [bendamustine, rituximab]. What those were is 63% of patients at 36 months or 3 years had a progression-free survival benefit, vs only 21% of patients in that combination, of either IdR or BR, and the P value of that was statistically significant, as I also mentioned.
In addition to that, what’s notable is that the PFS benefit was also consistent in high-risk subgroups. So that did also include those patients with deletion 17p, and we know that in CLL that’s one of the most common things that we have to look at in terms of prognostic criteria, also outside of IGHV, as Dr Perissinotti had mentioned. Now, in terms of the AEs [adverse events] that were observed in ASCEND, it really didn’t surprise us. What we would see with BR, chemoimmunotherapy, we saw. What we see with IdR, we saw. And what we see with acalabrutinib, we typically saw. As we know that with acalabrutinib, for example, headaches tend to be a problem. So all grade AEs around the headache with acalabrutinib was about 23%. Neutropenias were about 23%, also a BTK adverse event that’s common. With idelalisib and rituximab, for example, we did see more GI [gastrointestinal] adverse effects; about half of those patients had some type of diarrhea or a colitis component. About half of those patients also had neutropenias, and then with BR also hematologic adverse events were notable.
There were also some additional data reported for zanubrutunib. This was one of the early phase 2 studies looking at zanubrutunib in the relapsed/refractory CLL patient population. That phase 2 trial was one of the very first looking to see if zanubrutunib is effective in our CLL patient population, which one would think so. And these patients ultimately in the relapsed/refractory setting were on treatment until progression or unacceptable toxicity. In this phase 2 trial, about 91 patients were enrolled, 82 of these patients had CLL, and 9 had SLL [small lymphocytic lymphoma]. This was a study that primarily took place in China, not that there’s anything important that we wouldn’t be able to extrapolate, that wouldn’t apply to any other type of patient population. But again, based on just the company and where it originally started, and the large presence the company has had in China, this study was predominantly in China. And these patients had all types of prognostic criteria, deletion 17p, IGHV mutated and unmutated status.
What we initially saw in this trial was that about 7% of these patients had a CR [complete response], 70% had a PR [partial response], and the event-free rates or the progression-free survival incidences at 24 months, about 80.5% of patients had PFS benefit. Even looking at that at 36 months, because this was titled the 34-month readout, 68% of those patients did continue to benefit from zanubrutinib.
Transcript edited for clarity.
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.