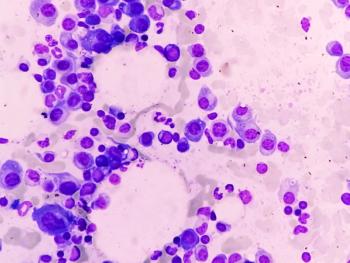
Multiple Myeloma
Latest News
Latest Videos
CME Content
More News
Risk stratification remains a challenge when selecting patients for treatment of smoldering multiple myeloma.

The 75 minutes of infusion time typically required is costly and difficult for patients.
C. Brooke Adams, PharmD, BCOP, discusses the evolving diagnostic criteria and management strategies for cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) in CAR T-cell therapy, highlighting advances in toxicity prevention and treatment selection.

OPN-6602 is an oral EP300/CBP bromodomain inhibitor that yielded 100% tumor regression as a combination therapy in mouse models.
The quadruple treatment was active and safe as initial therapy for older patients with transplant-ineligible multiple myeloma.
Ming-Hei Tai, PharmD, BCOP, shares his concerns about the AQUILA trial and use of daratumumab for smoldering multiple myeloma.

Expert weighs in on data from the AQUILA trial and Johnson & Johnson's approval request for daratumumab for smoldering multiple myeloma.
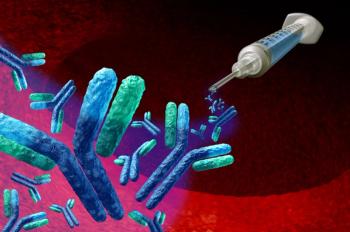
Isatuximab is a CD38-targeting monoclonal antibody that has demonstrated significant clinical success in improving minimal residual disease rates and progression-free survival.
Managing bispecific antibodies requires collaboration and meticulous protocols.
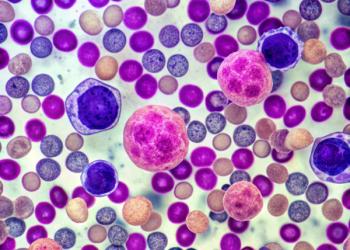
The international cohort study evaluated the safety, efficacy of BCMA-targeting agents ciltacabtagene autoleucel and idecabtagene vicleucel.

The combination yields promising results but was associated with high incidence of toxicity and infection.
The analysis shows patients achieved deep and durable responses despite being ineligible for the CARTITUDE-1 trial.
Patients with relapsed, refractory disease achieved deep, durable responses with equecabtagene autoleucel.

Panelists discuss how key recommendations for optimizing bispecific therapy care focus on establishing robust communication protocols between academic and community centers while ensuring community centers develop comprehensive infrastructure including staff training, emergency protocols, and care coordination pathways.

Panelists discuss understanding the comparative advantages, decision-making factors, infrastructure requirements, and partnership models for administering bispecific antibodies in community vs academic settings, with particular focus on patient care logistics and referral pathways.

Yi Lin, MD, PhD, highlights the importance of achieving MRD negativity in multiple myeloma, CAR T-cell therapy outcomes, and the critical role of pharmacists in patient care.
Emerging BCMA-Directed Therapies in Multiple Myeloma: Bispecific Antibodies and CAR T-Cell Therapies
Here is an updated overview of the role of BCMA-directed therapies following the 2024 ASCO Annual Meeting and EHA Congress.
The treatment landscape for multiple myeloma continues to evolve.

Panelists discuss the guidance on managing REMS program compliance for bispecific therapies and strategies for educating non-oncology health care providers about cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS) toxicities.

Panelists discuss insights on infection prevention protocols and electronic health record (EHR)–based toxicity management strategies for patients receiving bispecific antibody therapies in relapsed/refractory multiple myeloma (RRMM).

Panelists discuss how clinical management of CAR T-cell therapy–associated toxicities focuses primarily on early recognition and prompt intervention with tocilizumab and/or corticosteroids for cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS), following established grading systems and treatment algorithms.

Panelists discuss understanding institutional protocols for managing cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS) prophylaxis in bispecific antibody therapy, along with criteria for safely selecting patients for outpatient step-up dosing.
The phase 3 CEPHEUS trial demonstrated that adding daratumumab (DARA) to the VRd regimen significantly improves minimal residual disease negativity, progression-free survival, and overall response in transplant-ineligible or transplant deferred patients with newly diagnosed multiple myeloma, establishing a new standard of care.
The GMMG-HD7 trial evaluated the addition of isatuximab to standard induction therapy in patients with newly diagnosed multiple myeloma who are eligible for autologous stem cell transplantation, demonstrating significantly higher rates of minimal residual disease negativity and improved progression-free survival (PFS).
The AQUILA study demonstrates that early treatment with daratumumab significantly delays progression to symptomatic multiple myeloma, improves survival outcomes, and offers a well-tolerated alternative to traditional observation.