Educational Opportunities to Combat C. difficile Infection (CDI)
Drs. Lodise and Feuerstadt discuss educational opportunities to combat and reduce C. difficile infection (CDI).
Episodes in this series

Paul Feuerstadt, MD: Tom, we've covered a lot of information during this first section: C. [Clostridioides] difficile, anti-microbial stewardship, infection control, discussed elements of risk factors, and when to refer. Can you walk us through what education you think is most important for institutions to understand and teach each other with regard to C. difficile infection and recurrent C. difficile infection?
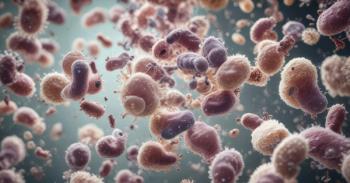
Thomas Lodise, PharmD, PhD: Sure. As Teena can attest, infection control, infection control, infection control. Follow best practices, and a very simple thing we can do is wash our hands. While I think we all become accustomed to using these alcohol-based hand sanitizers, you think about C. diff [Clostridioides difficile] as a sporulation disease, you have to wash your hands with soap and water for an adequate period of time, you know, 30 seconds. If you ever count to 30 seconds, it feels a lot longer than 30 seconds, but that is the single most important thing we can do to minimize the health care provider-to-patient transmission. As Teena mentioned, when these individuals go home, it’s important to minimize spread through households, or if they're going to some other long-term care facility. Another simple thing is to promote good gut health. We talk about this diet rich in fiber – it does make a difference. It can benefit in restoring and maintaining a hyper[ph] microbiome, it's a source of short-chain fatty acids. There are many positive benefits to a diet high in fiber. When we go beyond that, I think some of the modifiable risk factors, as you mentioned, (include) just looking at their medications. We think about antibiotics as everyday matters, so a lot of the time we do our stewardship, we spend more time getting individuals off antibiotics who do not need them, rather than broadening their antibiotics or even looking to narrow the spectrum. That suggests half the people in the hospital are on an antibiotic at any given point of time and 30% to 50% are inappropriate or unnecessary. So, there's a clear opportunity for stewardship and we think about support for stewardship programs in our hospital, avoidance of CDI is number 1, this supports all stewardship programs. Another simple thing, does that patient need the proton-pump inhibitor? Why is that still on? Do they need all these NSAIDs [non-steroidal anti-inflammatory drugs]? There is some opportunity where we start somebody as acute med, and they become chronic meds, and even we interview some of our patients at the hospital, "How long have you been taking your proton-pump inhibitor?" "Oh, 5 years." "Do you know why you're taking it?" "No." Always look for opportunities to look at somebody's drugs that promote dysbiosis. Then, finally, and this might sound counter-intuitive, prophylactic use of oral vancomycin in someone who is at risk for CDI. I know it's a very controversial topic, but I think what we have seen with the later clinical trial data, some of the iterations of the later CDI guidelines, it's a broad-spectrum agent that creates an environment of dysbiosis. Sometimes when we think we're helping our patients, we're actually doing the exact opposite than what we're trying to obtain. Some simple things are washing your hands, promote good gut health, then looking at their medications, take medications off, and practice stewardship. As Teena mentioned, they're on antibiotics a couple of days, they could have a dysbiosis for 3 months, if not longer. With the fluoroquinolones, we see it even longer than that. Clearly, stewardship has a major role in minimizing C. diff in our patients.
Paul Feuerstadt, MD: I agree completely with everything that you said. It's important that we understand that. In July, obviously, we have the new residents in; almost all patients that show up in the emergency room get on a bowel regimen and a PPI [proton-pump inhibitor] for whatever reason. The PPIs stay on forever, the bowel regimen stays on until the patients get diarrhea, and then they'll get checked for C. difficile, and then we know what happens after that, right? It's really thinking our way through this but also understanding, as you pointed out, that alcohol-based hand sanitizers do not destroy the spore phase. The spore phase is really hardy; there was a really interesting study that was performed in Britain a couple of years ago, and they looked at the volume of the spore phase on bedsheets from individuals who had C. difficile. They looked at precleansing versus postcleansing with a sodium hypochlorite or acetic acid solution. You know what? Precleansing it was 51 colony forming U/cm^2; post, it was 33 U/cm^2. They were still there even though a standard cleansing agent was used, essentially, bleach. We need to understand that there's so many different ways, and so many different things that we can educate on, to minimize the spread and minimize the risk.
Transcript edited for clarity
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.