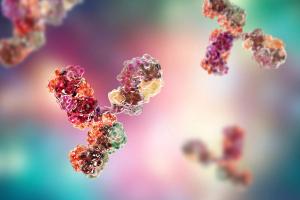
The FDA approves zanidatamab for HER2-positive biliary cancer, improving treatment options.
The FDA approves zanidatamab for HER2-positive biliary cancer, improving treatment options.
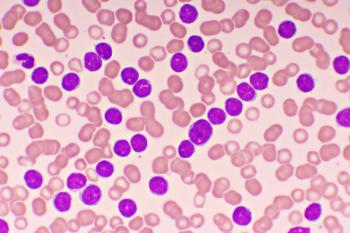
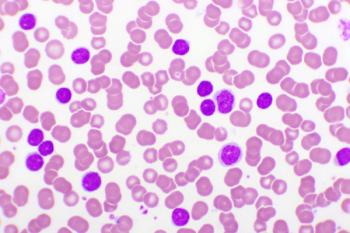
Obecabtagene autoleucel improves CAR T-cell therapy for B-cell ALL.

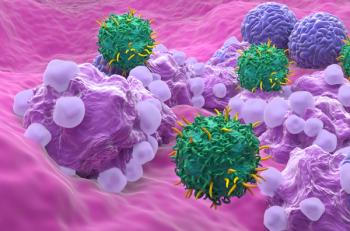
Amir Ali, PharmD, BCOP, and Allison Hsieh, PharmD share insights from their presentation about cytokine release syndrome, ICANS, and CAR T-cell therapy.

Amir Ali, PharmD, BCOP, discusses his experience as an oncology pharmacist in both direct and indirect patient care at the University of Southern California (USC) Norris Comprehensive Cancer Center.
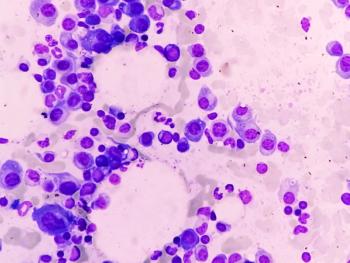
Here is an updated overview of the role of BCMA-directed therapies following the 2024 ASCO Annual Meeting and EHA Congress.

The panel discussion concludes with final thoughts on the future landscape of newly diagnosed multiple myeloma.

Panelists discuss how pharmacists can address remaining unmet needs and challenges in optimizing frontline therapy for patients with transplant-eligible newly diagnosed multiple myeloma (NDMM), including areas such as managing complex drug interactions, improving medication adherence, mitigating treatment-related toxicities, streamlining transitions of care, and enhancing patient education and support throughout the treatment journey.

Panelists discuss how they navigate challenges with payer coverage for quadruplet regimens in multiple myeloma treatment, including strategies they employ to address insurance denials or restrictions, such as providing clinical justification, leveraging recent trial data, and collaborating with financial assistance programs to ensure patients can access optimal therapy despite potential coverage difficulties.

Panelists discuss how treatment regimens for multiple myeloma patients can be personalized to improve adherence and quality of life by considering factors such as dosing schedules and routes of administration while emphasizing the role of pharmacists in providing resources and support to keep patients informed, engaged, and compliant with their individualized treatment plans.

Panelists discuss how pharmacists actively engage in educating and coordinating with nurses, oncologists, and other health care providers by conducting in-service trainings, participating in multidisciplinary team meetings, and collaborating on the development and implementation of formularies, order sets, and treatment protocols to ensure optimal patient care in multiple myeloma management.

Panelists discuss how pharmacists play a crucial role throughout the multiple myeloma patient journey, from diagnosis to treatment, by contributing to medication management, patient education, adverse effect monitoring, and the development and implementation of order sets and clinical pathways within electronic medical record systems, thereby enhancing treatment efficacy and patient safety.

Panelists discuss how subcutaneous (SC) administration of drugs like daratumumab offers advantages over intravenous (IV) administration in terms of reduced health care resource utilization, improved patient convenience, and potentially better treatment adherence, while also considering potential drawbacks such as injection site reactions and the need for proper training in SC administration techniques.

Panelists discuss how the FDA approval of daratumumab and hyaluronidase-fihj combined with VRd (bortezomib, lenalidomide, and dexamethasone) for induction and consolidation in transplant-eligible newly diagnosed multiple myeloma patients is changing treatment approaches while also considering how recent evidence suggesting reduced observation time for subcutaneous (SC) daratumumab administration may streamline patient care and improve treatment efficiency.

Panelists discuss how recent phase 3 trial data from PERSEUS, IsKia, and GMMG HD7 are shaping their approach to induction and consolidation therapy in transplant-eligible newly diagnosed multiple myeloma (NDMM) patients, particularly focusing on the incorporation of CD38 antibodies into upfront treatment regimens and the potential shift from triplet to quadruplet therapies based on these pivotal trial findings.
The therapy offers new hope in solid tumor treatment with fewer adverse effects.

Panelists discuss how implementing novel combination therapies or emerging agents from clinical trials into real-world clinical practice for multiple myeloma faces significant challenges, including managing complex dosing regimens, addressing potential toxicities, ensuring patient adherence, navigating insurance coverage and cost issues, and bridging the gap between highly controlled trial conditions and diverse patient populations encountered in everyday clinical settings

Panelists discuss how a new therapy for multiple myeloma would need to demonstrate significant improvements in efficacy, safety, or quality of life over current standards of care to warrant adoption while also considering factors such as cost-effectiveness, patient preferences, and ease of administration in their decision-making process for evaluating treatment changes.

Panelists discuss how clinical trials in multiple myeloma can be improved to better reflect real-world scenarios and patient outcomes, emphasizing the importance of end points such as progression-free survival, overall survival, and quality of life measures, while also considering ways to increase trial inclusivity and applicability to diverse patient populations.

Panelists discuss how the introduction of triplet therapy prior to transplant in studies like IFM 2009 and DETERMINATION shifted the clinician mindset toward more intensive induction regimens, leading to a focus on achieving deeper responses and longer progression-free survival as primary goals of therapy for newly diagnosed multiple myeloma patients.

Panelists discuss how various patient characteristics, including age, fitness level, cytogenetic risk, and comorbidities, influence their decision to use more intensive quadruplet regimens like D-VRd (daratumumab plus bortezomib, lenalidomide, and dexamethasone) vs standard triplet regimens, such as VRd or KRd (carfilzomib, lenalidomide, and dexamethasone) in transplant-eligible multiple myeloma patients, while also considering administration logistics and supportive care requirements

Panelists discuss how transplant eligibility significantly influences first-line treatment goals and initial therapy selection in multiple myeloma, often leading to more intensive induction regimens aimed at achieving deep remissions.

Panelists discuss how their institutions approach frontline treatment for transplant-eligible multiple myeloma patients, typically using a combination of novel agents like proteasome inhibitors and immunomodulatory drugs, followed by autologous stem cell transplantation and maintenance therapy, while considering factors such as patient characteristics and treatment response to guide therapy sequencing.

Panelists discuss how the current first-line treatment options for transplant-eligible patients with newly diagnosed multiple myeloma (NDMM) typically involve combination therapies including proteasome inhibitors, immunomodulatory drugs, and steroids.
Pharmacists play a vital role in therapy selection.

The significant surge in oncology drug shortages in 2023 particularly affected essential chemotherapeutic drugs.
Treatment options are distinct in their mechanisms, safety profiles, and implications for patients’ quality of life.
Ph-like ALL may be predominantly prevalent in Hispanic and Latino populations.
In crafting a patient-centered regimen, the convergence of expertise from physicians and pharmacists, paired with the values and preferences of patients, becomes paramount.

A single-center experience at a tertiary medical center precision medicine clinic provides insight.
Achieving MRD flow cytometry negativity is crucial in monitoring and predicting survival outcomes.
Published: April 12th 2023 | Updated:

Published: April 10th 2025 | Updated: