Myelofibrosis
Latest News
FDA Grants Orphan Drug Designation to Zavabresib for the Treatment of Myelofibrosis
Latest Videos
CME Content
More News

Ropeginterferon alfa-2b shows promising results in treating preprimary myelofibrosis, enhancing clinical responses and safety in patients.
INCB057643 shows promise in treating myelofibrosis, enhancing anemia and symptom relief.
Explore the latest advancements in myelofibrosis treatment, focusing on JAK inhibitors and pegylated interferons for improved patient outcomes.

Imetelstat shows promise in treating myelofibrosis, enhancing survival, and modifying disease biology in patients resistant to JAK inhibitors.

The combination demonstrated improved efficacy compared with ruxolitinib as a monotherapy.


Patients with myelofibrosis who stopped ruxolitinib on the first day of conditioning did not show higher rates of acute graft-vs-host disease (GVHD).

Explore the role of JAK inhibitors in myelofibrosis treatment, focusing on optimizing dosages and managing adverse effects for better patient outcomes.

Thrombosis occurs in approximately 20% of myeloproliferative neoplasms.

Real-world data support momelotinib as an effective and well-tolerated treatment for myelofibrosis-related anemia.
Current treatment strategies are aimed at reducing hematocrit and symptom burden through phlebotomy, aspirin, and cytoreductive agents, while emerging therapies offer promise for better disease control and quality of life.
The trial showed that adding pelabresib to ruxolitinib improved outcomes in myelofibrosis with manageable adverse effects.
Interim results from an observational trial of patients with myelofibrosis indicate upward trends in health-related quality of life when started on the highest tolerable dose of ruxolitinib.
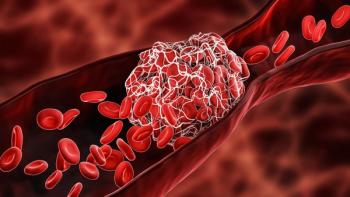
Using Janus kinase inhibitors, having experienced a previous thrombosis episode, and higher age were associated with a heightened risk of a new thromboembolic event.

Allogeneic stem cell transplant (allo-SCT) conditioning with busulfan/fludarabine with thiotepa and posttransplant cyclophosphamide induced improved 2-year progression-free survival and overall survival in patients with myelofibrosis, especially older adults.
Treatment with ruxolitinib in patients with myelofibrosis and anemia was associated with more inpatient medical center and emergency department visits while increasing health care-related financial burdens compared with nonanemic patients.
Measures including disease-free survival and overall survival were improved in patients with MF who underwent hematopoietic stem cell transplantation (HSCT) and a 3D volumetric splenomegaly analysis.

At 1- and 2-year follow-up points, ruxolitinib led to considerable improvements in survival in patients with myelofibrosis who develop graft-versus-host disease (GVHD).
Even for patients with myelofibrosis who could otherwise proceed directly to hematopoietic cell transplantation, pre-transplant treatment with ruxolitinib led to improved survival benefits.

Using chromosome genomic array testing in combination with existing risk stratification models can better determine patients with myelofibrosis who can benefit from transplant.

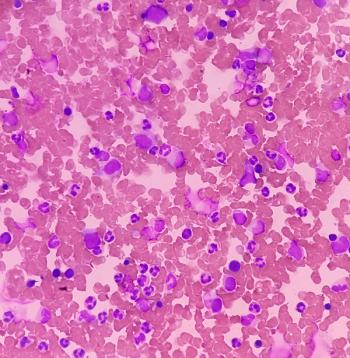
Cytopenic myelofibrosis is characterized by poorer prognosis and more severe anemia and thrombocytopenia compared with proliferative myelofibrosis.

Circulating lactate is increased in patients with myelofibrosis and corresponds with the remodeling of lactate export channel monocarboxylate transporter 4, suggesting a link with fibrosis establishment.

More accurate prognostic risk assessment could aid pharmacists in the management and counseling of patients with primary myelofibrosis.

Myelofibrosis patients with CALR mutations have lower responses to symptoms and higher rates of anemia after 6 months of therapy with ruxolitinib.

Diagnosing anemia, a serious and common complication of patients with myelofibrosis, could be made easier with the use of red cell distribution width assessment.